 Occupational Therapy Gives a Smile for Life
Occupational Therapy Gives a Smile for Life
FLOTEC submission
Julie M Bezold, OTD, OTR/L
Julie Hamel Veith, OTR/L
Trending topics in Occupational Therapy (OT) practice that align with accreditation standards put forth by Accreditation Council for Occupational Therapy Education (ACOTE) include the role of promotion of health and prevention, social determinants of health, and interprofessional collaboration. What better way for OTA students to become familiar with these trends than learning from and with dental hygiene students by communicating the distinct nature of occupation while promoting oral health and prevention.
Oral health remains one of the most prevalent unmet health needs among children in the United States. Early childhood caries (ECC), or dental cavities, is the most chronic disease of childhood affecting approximately half of the children eleven years old and younger in the United States (Martin et al., 2018). Dental caries leads to physical and psychosocial problems, pain, school absenteeism, concentration issues, obesity, cardiac and respiratory issues, diabetes, and poor oral health as an adult (Mahat & Bowe, 2017). ECC is preventable when caregivers implement strategies consistent with good preventative dental care and daily oral hygiene routine. Unfortunately, these preventative services are underutilized due to caregivers’ lack of knowledge or access to such services. In some cases, a child’s difficulty with processing sensory input can also affect oral hygiene routines in the home and in the dental office. Even when caregivers follow good oral health habits at home, professional dental visits are required for prevention and treatment. Dental care providers are generally not accessible or affordable for low socioeconomic status individuals or families or don’t accept low-income insurance (Biordi, 2015). Medicaid typically is the provider for these individuals and often places a cap on the number of clients that services are provided to (Verlinden et al., 2019). Other barriers affecting oral health outcomes include social determinants of health, parent education, cultural beliefs, values, and attitudes, family structure, access to transportation, and current health status (Healthy People 2020, n.d.). Social determinants of health which are “conditions in the environments in which people live, learn, work, play, worship, and age that affect a wide range of health, functioning and quality of life (healthy people 2020,n.d). Access to nutrition, housing, clean water, employment, healthcare, and education are examples of social determinants of health that play a role in oral health outcomes (Healthy people 2020, n.d.).
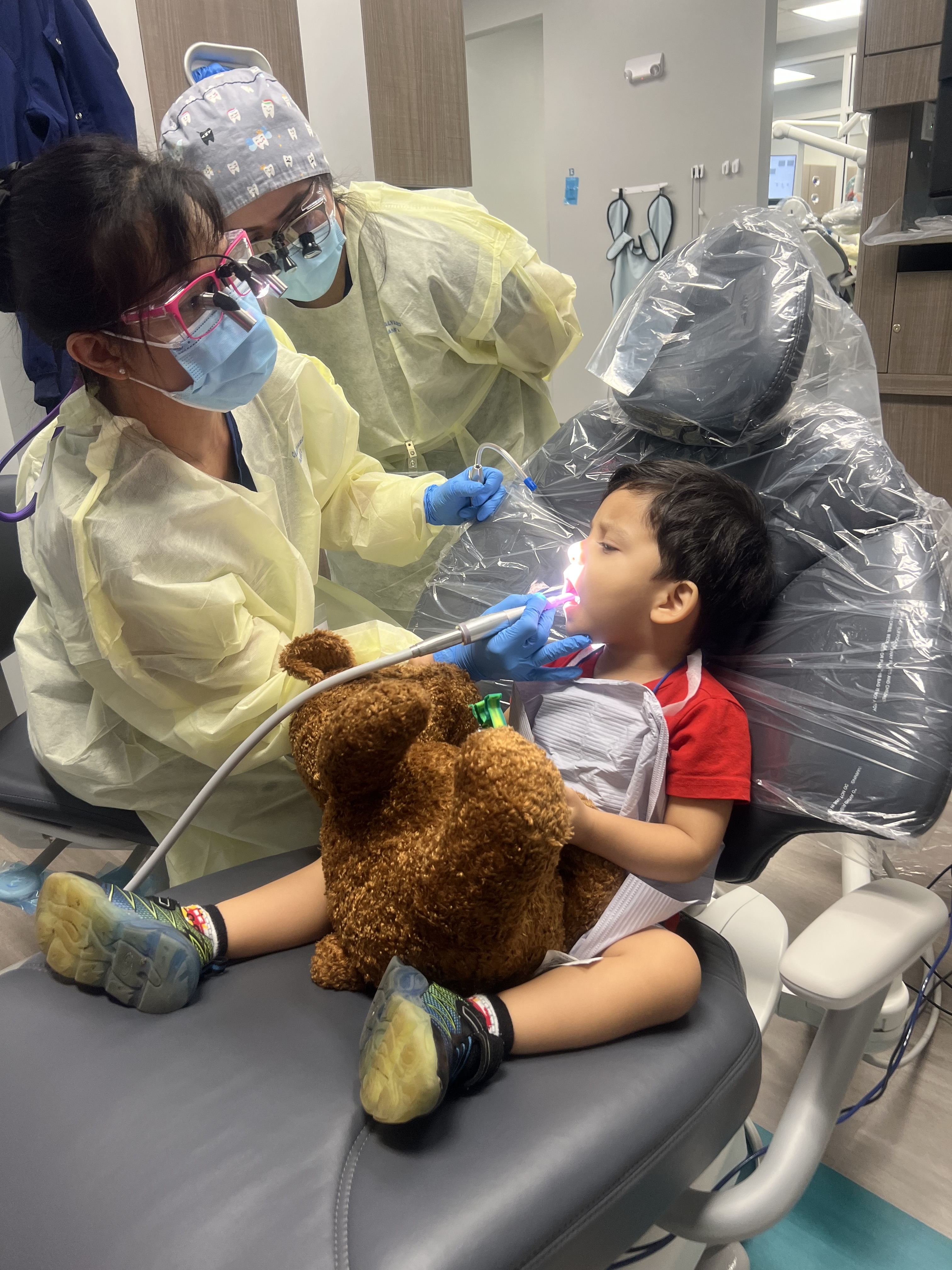
OT scope of practice includes not only oral hygiene, but also supports individuals in building positive habits and routines to promote health and wellness (AOTA, 2020b). OT practitioners have the training and unique skill sets to address the relationship between oral health behaviors, sensory integration, provide behavior management strategies, techniques to promote daily oral hygiene habits and routines, and collaborate with other professionals to provide client-centered care through meaningful activities. OTs specialize in modifications to environments and tasks to promote participation and improve the overall oral hygiene experience which is essential in fostering self-management skills in health promotion. Common barriers for children in oral care that align with OT education and training include sensory needs, behavioral challenges, and environmental barriers. Children with sensory needs may exhibit discomfort with textures of gloves or taste of the toothpaste, loud noises, the pressure of the bristles on the toothbrush, temperatures, bright lights, odors, or even vestibular experiences such as leaning back in the dental chair. OTs can create a sensory friendly environment to promote emotional regulation while receiving oral health care. Sensory strategies include providing noise cancelling earphones, sunglasses, weighted stuffed animals or blankets, music to listen to, vibrating toothbrushes, chewy sticks prior to the appointment, and fidgets during the appointment. Behavioral challenges are addressed by visuals, reward systems such as stickers, toys, social stories to prepare for appointments to familiarize the child with what to expect, or the use of distractions such as watching a movie.
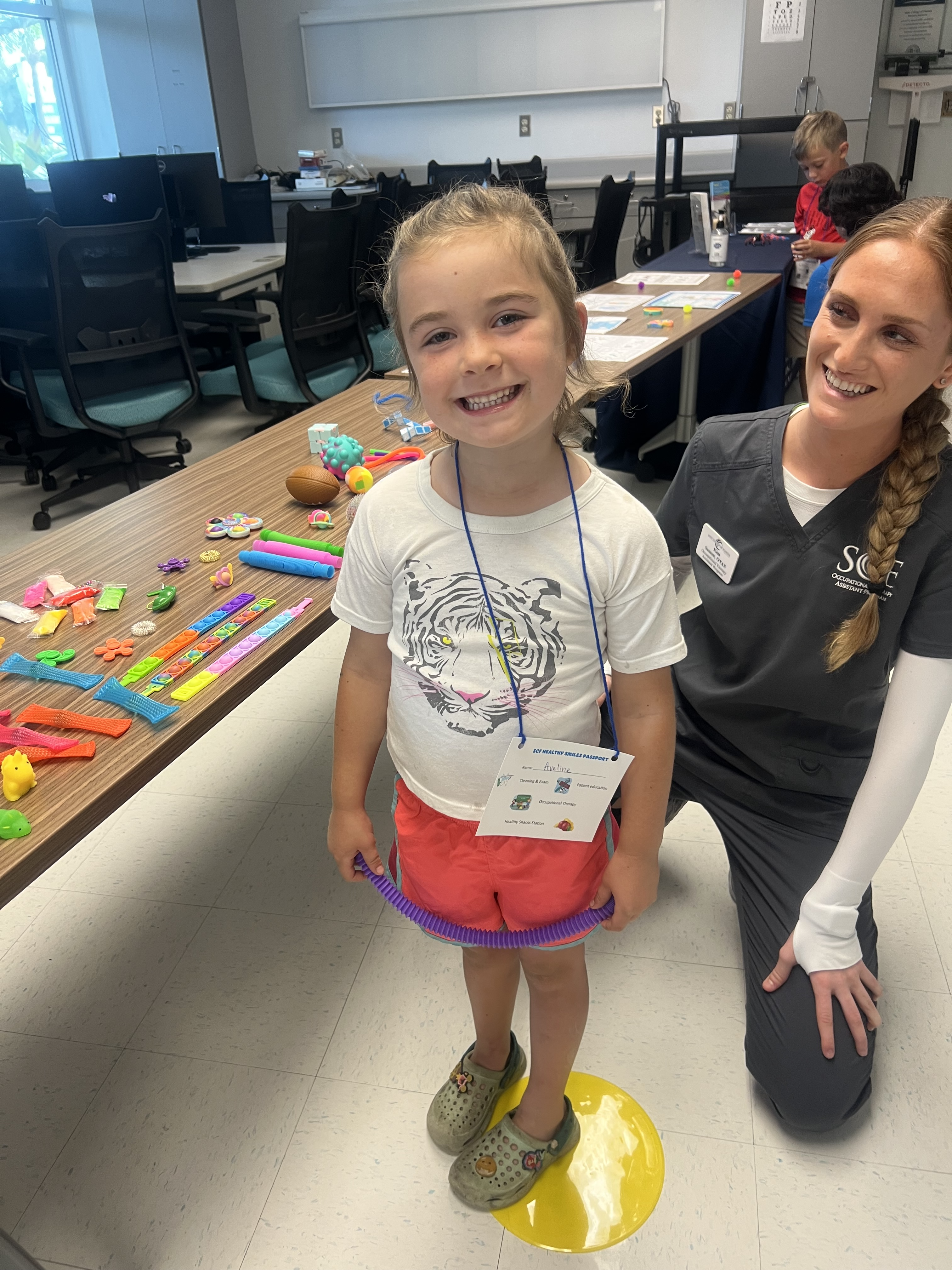
OTA and dental hygiene students at State College of Florida (SCF), participated in an oral care event offering free education and training to local elementary schools composed primarily of underserved populations. These services made available through a grant allowed preventative dental care for persons from Kinderdargarten through twelfth grade at SCF’s Dental Clinic. Through this grant, interprofessional team members were provided the tools to offer education and care to individuals who may never have been exposed to dental or occupational therapy services. OTA and dental hygiene students worked together utilizing strengths from each team member to effectively address the oral health of children and provided necessary interventions to meet the oral health care needs of underserved populations. Children and their families arrived at SCF at their scheduled appointment time and participated in various oral education modules. Dental hygiene students, faculty, and staff alternated between stations consisting of dental exams, cleanings, x-rays, fluoride treatments, nutrition, and oral education. OTA students created a sensory station consisting of weighted toys, calming lights, fidget toys, proprioceptive activities and other sensory regulating activities making it easier to tolerate oral hygiene activities. Social stories were fabricated to prepare participants of the expectations and sequencing during the exam as well as how to incorporate healthy routines. OT faculty and students performed screenings and questionnaires to assess potential sensory processing deficits and provide suggestions for adaptive aids to increase skills and abilities during oral hygiene. All children participating in this interprofessional collaboration activity received an electric toothbrush, toothpaste, a two-minute sand timer, dental floss, and a healthy food snack pack. Each child had the opportunity to choose a fidget to use as a distractor as needed during the dental examination.
According to the OTPF 4th Ed., working with individuals, groups, and population’s related to establishing and promoting routines, habits, and roles to successfully implement health and wellness behaviors into their lives is within OTs scope of practice, so it is fitting that it be addressed in holistic care through an interprofessional collaboration event to promote children’s oral health (AOTA, 2020a).


References
Accreditation Council for Occupational Therapy Education [ACOTE]. (2018). Accreditation Council for Occupational Therapy Education (ACOTE®) standards and interpretive guide. https://acoteonline.org/accreditation-explained/standards/
American Occupational Therapy Association (2020a). Occupational therapy practice framework: Domain and process, (4th ed.). American Journal of Occupational Therapy, 74 (Suppl.2.).
American Occupational Therapy Association (2020b). Role of occupational therapy in primary care. American Journal of Occupational Therapy, 74
Anderson, K., Anderson, T., Bendelsmith, E., Despres, B., Howe, C., Leaser, J., Minor, E., Sandler, D., & de Sam Lazaro, S.L. (2020). Providing oral health education to underserved children and families within an interdisciplinary team [Master’s project, St. Catherine University]. https://sophia.stkate.edu/ma_osot/
Biordi, D.L., Heitzer, M., Mundy, E., DiMarco, M., Thacker, S., Taylor, E., Huff, M, Marino, D., & Fitzgerald, K. (2015). Improving access and provision of preventive oral health care for very young, poor, and low income children through a new interdisciplinary partnership. American Journal of Public Health, 105(5, Suppl. 2), 23-29.
Health People. (2020). Social determinants of health. https://www.healthpeople.gov/2020/topics-objectives/topic/social-determinants-of-health
Health People. 2020. (n.d.). Disability and health. https://www.healthypeople.gov/2020/topicsobjectives/topic/disability-and-health
Mahat, G., & Bowen, F. (2017). Parental knowledge about urban preschool children’s oral health risk. Pediatric Nursing. 43(1), 30-34.
Martin, M., Frese, W., Lumsden, C., & Sandoval, A. (2018). Building a pediatric oral health training curriculum for community health workers. Journal of Public Health Management Practice, 24(3), 9-18.
Verlinden, D.a., Reijneveld, S.A,, C.I., Wouwe, J.P., & Schuller, A.A. (2019). Socio-economic inequality in oral health in childhood to young adulthood, despite full dental coverage. European Journal of Oral Sciences, 127(3), 248-253,
